DELIVERY SYSTEM REFORM INCENTIVE PAYMENT PROGRAM (DSRIP)
We successfully led the implementation of the very complex DSRIP Program. The program improved the design and delivery of healthcare for the Medicaid population by reducing avoidable hospitalization and improving population health, while lowering the cost of healthcare.
DSRIP
Clinical Quality Outcome Improvement Program
A key tenet of our mission is the improvement of population health outcomes. Over the course of the DSRIP program, our partnership network improved performance in nearly 40 clinical outcome measures across the region, with significant achievements in several domains including behavioral health outcomes, long-term care, patient satisfaction, and maternity and children’s measures. Understanding that population health improvement requires cohesive participation by all Partners, we focused on a region-wide approach to clinical outcome improvement.
Mid-DSRIP, we developed a strategy and implementation plan that would improve health outcomes quickly and significantly, via activities performed that would supplement the ongoing DSRIP projects.
Our Clinical Quality Committee (CQC) collectively examined specific characteristics of each clinical outcome metric and categorized the metrics into various categories for targeted improvement activities.
The Sprint
CQC led an innovative program referred to as the “Sprint” to improve performance quickly, given that there were only three months remaining in the year four measurement period (MY4).
91%
of the improvement targets were met or exceeded
The Jog
We initiated the “Jog” at the beginning of year five measurement period (MY5) and engaged additional partners including community-based behavioral health organization networks and Health Home as these provider types would be critical in accomplishing improvement in behavioral health outcome metrics.
95%
of the improvement targets were met or exceeded
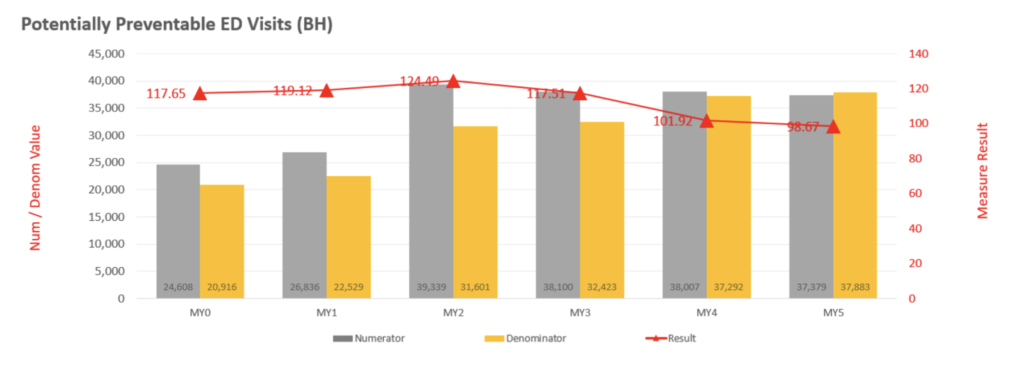
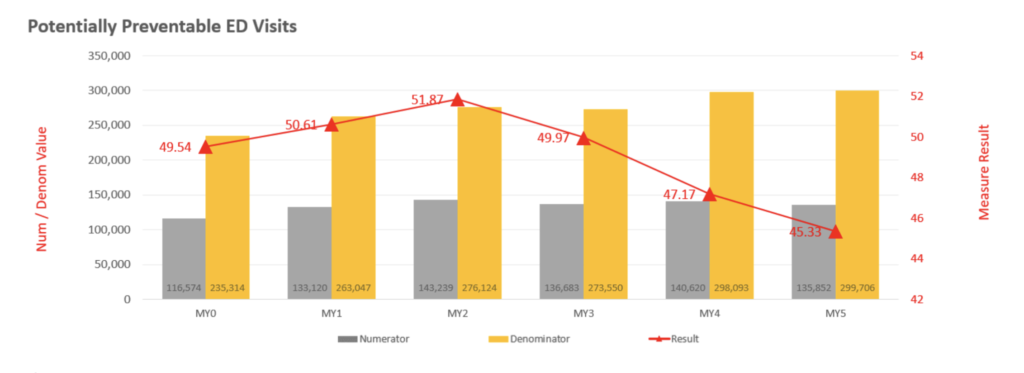
The graphs above illustrate the overall success in the Sprint and the Jog in reducing preventable ED use, both within the overall Medicaid population and those specifically with a behavioral health condition. These health outcome improvements came about through the vision and collaborative efforts of our team, the CQC and partnering organizations, cohesively working together towards the common goal of improving the health outcomes of the most vulnerable in our region.
“For decades Regional Health Reach has been a leader in the community in providing healthcare and support services to those experiencing homelessness. Through our traditional clinic, mobile medical unit, and presence at shelters, our Healthcare for the Homeless program has touched thousands of lives. Health Reach is excited to partner with Finger Lakes Performing Provider System and MC Collaborative to expand our reach to unsheltered individuals, meeting them where they are, to provide the care they need.”
“By expanding our Person In Crisis teams to include certified peer specialists, we will be able to assist even more of our residents in need in a humane and compassionate manner. In addition, by assisting residents in this new way, we are expecting that there will be a reduced number of people calling the PIC team because they are getting connected to the services they need.”
“The key to the success of this menu of services is our ability to have a two-way dialogue with doctors and other medical professionals about both health and social support needs at home. We’ve proven this model can improve patient outcomes and reduce unnecessary ED visits and hospitalizations, and that’s a win for everyone. It also reduces both physician and patient/family caregiver frustrations.”
“I am excited to see ‘equity in action’ through this partnership with FLPPS, who recognizes the importance of lived experience and elevating the parent and patient voice to bring change across our health and behavioral health systems.”
“The Finger Lakes IPA, a partnership of the region’s community health centers, six behavioral health organizations, and the S2AY Rural Health Network, is very excited to be a part of this important initiative by FLPPS to support the critical need for access to developmental screenings for young children in our rural communities. This program will give us the ability to provide access to services that are often not available due to geographic and other barriers to care experienced by our patients.”

